Prostate Cancer, Advanced or Metastatic
Condition Basics
What is advanced or metastatic prostate cancer?
Prostate cancer is the abnormal growth of cells in the prostate gland. The prostate is part of the male reproductive system. Locally advanced prostate cancer means that the cancer has spread beyond the prostate and into nearby tissue. Metastatic prostate cancer means that the cancer has spread, or metastasized, to the lymph nodes or other parts of the body.
Recurrent prostate cancer means that the cancer has come back after it was treated. The cancer can come back in the prostate. Or it can come back near the prostate or in another part of the body. If it comes back in another part of the body—often the bones—it is still called prostate cancer because it started in the prostate.
What are the symptoms?
Possible symptoms of locally advanced prostate cancer may include trouble urinating or pain when you urinate. Symptoms of metastatic prostate cancer may include bone pain, weight loss, or swelling in your legs and feet. Sometimes there are no symptoms of locally advanced or metastatic prostate cancer.
How is it diagnosed?
Advanced and metastatic prostate cancer are diagnosed using a combination of a physical exam, blood tests, imaging tests, and sometimes biopsies. If you've had prostate cancer before, you'll likely be having regular PSA tests. Other tests to see if the cancer has come back or spread include bone scans, PET-CT scans, and MRI scans.
How is advanced or metastatic prostate cancer treated?
Advanced or metastatic prostate cancer may be treated with hormone therapy, radiation therapy, chemotherapy, targeted therapy, or immunotherapy. Some of these treatments may be combined. Other options may include surgery or observation. For either type of cancer, your doctor may suggest a clinical trial.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
Symptoms
Sometimes there are no symptoms of locally advanced or metastatic prostate cancer.
When there are symptoms of locally advanced prostate cancer, they may include urinary problems, such as:
- Not being able to urinate at all.
- Having a hard time starting or stopping the flow of urine.
- Having to urinate often, especially at night.
- Having pain or burning during urination.
Less common symptoms of locally advanced prostate cancer may include:
- Difficulty having an erection.
- Blood in your urine or semen.
- Deep and frequent pain in your lower back, belly, hip, or pelvis.
These symptoms also may be caused by an enlarged prostate, an infection in the prostate (prostatitis), or a urinary tract infection.
Symptoms of metastatic prostate cancer may include:
- Weight loss.
- Bone pain.
- Swelling in the legs and feet.
What Happens
Prostate cancer is usually a very slow-growing cancer. It may take years to grow large enough to cause any symptoms. Sometimes it never causes problems. But sometimes it grows quickly and may cause complications or death.
Prostate cancer may grow beyond the prostate and into nearby tissues, such as the nearby seminal vesicles. This is called locally advanced prostate cancer.
Prostate cancer may spread to the lymph nodes or other parts of the body. This is called metastatic prostate cancer. Most often, prostate cancer spreads to the bones. It also may spread to the lungs or other organs.
Progression of prostate cancer
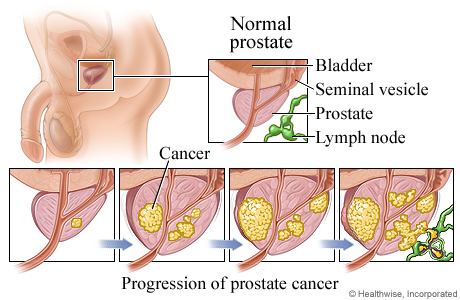
Prostate cancer begins inside the prostate gland. Usually this cancer grows so slowly that it may never cause a problem during a person's life. But in some cases, it grows more quickly, spreading into nearby tissues, such as the lymph nodes or seminal vesicles, and to other areas of the body.
When to Call a Doctor
Be sure to follow your doctor's instructions about calling when you have problems, new symptoms, or symptoms that get worse.
Call your doctor now if you:
- Are completely unable to urinate.
- Have painful urination and a fever, chills, or body aches.
- Have blood or pus in your urine or semen.
Call your doctor to schedule an appointment if you have unexplained:
- Weight loss.
- Dull, aching pain in your lower back, pelvis, or hips.
- Swollen lymph nodes in the groin area. These nodes are usually not tender.
Watchful waiting
Watchful waiting is a wait-and-see approach. If you are older and have other serious health problems, you may choose only those treatments that keep you comfortable (palliative care).
Exams and Tests
Locally advanced and metastatic prostate cancer are diagnosed through physical exams and tests. These include:
- A digital rectal exam.
- Blood tests, including a PSA test. A rising PSA level after treatment for prostate cancer can mean your cancer has come back.
- Imaging tests, such as:
- A transrectal ultrasound.
- An MRI called a multiparametric MRI (mpMRI). It provides detailed information about the prostate.
- A CT scan or a PET-CT.
- A bone scan.
- A prostate biopsy.
- Genetic tests. These include tests to look for inherited gene changes and tests that look for biomarkers.
If you've had prostate cancer before, other tests can help your doctor see if your cancer has come back or spread. These tests may include:
- PSA tests to check the PSA levels in your blood.
- Imaging tests, such as a bone scan, CT scan, MRI, and PET-CT.
- Biopsies of lymph nodes, bones, or other tissues where the cancer may have spread.
Learn more
Treatment Overview
Treatment for advanced prostate cancer is based on the stage of the cancer, your Gleason score, and other things, such as your age and overall health. It may include:
- Hormone therapy.
- This uses medicine or surgery to lower the level of androgens in your body. This can slow the growth of prostate cancer and even shrink the tumors. It may also be called androgen deprivation therapy (ADT).
- Radiation therapy.
- This uses high-dose X-rays to destroy cancer cells and shrink tumors. It may be given to treat the cancer or to help relieve symptoms.
- Surgery.
- The doctor may remove the prostate. This is called radical prostatectomy.
- Chemotherapy.
- These medicines kill fast-growing cells, including cancer cells and some normal cells.
Other treatment options may include targeted therapy or immunotherapy. In some cases, a clinical trial may be a good choice.
Your doctor will talk with you about your options and then make a treatment plan.
Treatment for metastatic prostate cancer
Treatment for metastatic prostate cancer is based on many things. These include your age and overall health, the location of the cancer, and whether you had treatment before. Options may include hormone therapy, radiation therapy, chemotherapy, targeted therapy, and immunotherapy. These treatments may be combined. Your doctor may suggest a clinical trial.
Your doctor will talk with you about your options and then make a treatment plan. Some people choose to focus on treating their symptoms instead of the cancer (observation).
Some people use complementary therapies along with medical treatment. Therapies like acupuncture or massage may help you cope with the symptoms and stress of cancer. Talk with your doctor about any of these options you would like to try.
Hormone therapy
Hormone therapy uses medicine or surgery to lower the level of androgens in your body. This can slow the growth of prostate cancer and even shrink the tumors. It's also called androgen deprivation therapy (ADT).
- If you aren't taking hormone therapy, you'll most likely start. You may take medicines that stop the body from making testosterone. These include LHRH agonists and LHRH antagonists.
- If you're already taking hormone therapy, you may keep taking it. But your doctor may add another hormone therapy. An example is abiraterone.
Medicines
Over time, hormone therapy may no longer keep the cancer from growing. This is called castration-resistant prostate cancer (CRPC). Hormone therapy may be continued, but other medicines are added. Examples include:
- Other hormone therapies.
- These include abiraterone, apalutamide, and enzalutamide.
- Chemotherapy.
- These medicines kill fast-growing cells, including cancer cells and some normal cells.
- Targeted therapy.
- These medicines target cancer cells and may cause less harm to normal cells. They help keep cancer from growing or spreading. They include PARP inhibitors, which may be an option for some people with metastatic prostate cancer who have certain gene changes, such as BRCA1 or BRCA2.
- Immunotherapy.
- This treatment helps your immune system fight cancer. One type is a cancer vaccine that's made from your own white blood cells.
Radiation therapy
This uses high-energy X-rays to kill cancer cells and shrink tumors. Radiation may be used to treat the cancer or to ease symptoms. It may be used alone or given with hormone therapy.
To treat prostate cancer, radiation is usually given by a machine outside the body. (This is called external radiation.) It may also be given by placing substances inside the body. (This is called internal radiation, or brachytherapy.)
Other treatments
These may include:
- Medicines that contain a radioactive substance.
- An example is radium-223. The medicine is given as a shot (injection). It's absorbed by the affected bone and releases the radiation. It may be used with hormone therapy to treat cancer that has spread to the bones (bone metastases). It also helps relieve pain caused by bone metastases.
- Medicines for bone problems.
- These may help relieve bone pain and prevent bone loss (osteoporosis). Osteoporosis is sometimes caused by long-term hormone therapy.
- Steroids.
- These medicines help control pain and improve appetite. Examples include hydrocortisone and prednisone.
Clinical trials
Clinical trials are an option for many people who have cancer. These research studies test promising new treatments or improvements to existing treatments. People in clinical trials may have access to the latest treatments before they're available to others.
Your medical team can tell you if there's a clinical trial that might be right for you.
Observation
This is a wait-and-see approach to treatment. You have regular visits with your doctor, but the focus is on treating any symptoms that bother you rather than treating the cancer. Some people choose this because it lets them avoid or delay treatments that can have serious side effects.
You can change your mind and start treatment at any time.
Learn more
Supportive Care
Palliative care is a type of care for people who have a serious illness. It's different from care to cure your illness, called curative treatment. Palliative care provides an extra layer of support that can improve your quality of life—not just in your body, but also in your mind and spirit. Sometimes palliative care is combined with curative treatment.
The kind of care you get depends on what you need. Your goals guide your care. You can get both palliative care and care to treat your illness. You don't have to choose one or the other.
Palliative care can help you manage symptoms, pain, or side effects from treatment. It may help you and those close to you better understand your illness, talk more openly about your feelings, or decide what treatment you want or don't want. It can also help you communicate better with your doctors, nurses, family, and friends.
End-of-life care
It can be hard to live with an illness that cannot be cured. But if your health is getting worse, you may want to make decisions about end-of-life care. Planning for the end of your life does not mean that you are giving up. It is a way to make sure that your wishes are met. Clearly stating your wishes can make it easier for your loved ones. Making plans while you are still able may also ease your mind and make your final days less stressful and more meaningful.
Learn more
Self-Care
- Take your medicines exactly as prescribed. Call your doctor if you think you are having a problem with your medicine.
- Follow your doctor's instructions to relieve pain. Pain from cancer and surgery can almost always be controlled. Use pain medicine when you first notice pain, before it becomes severe.
- Eat healthy food. If you do not feel like eating, try to eat food that has protein and extra calories to keep up your strength and prevent weight loss.
- Get some physical activity every day, but do not get too tired.
- Get enough sleep, and take time to do things you enjoy. This can help reduce stress.
- Think about joining a support group. Or discuss your concerns with your doctor or a counselor.
- If you are vomiting or have diarrhea:
- Drink plenty of fluids to prevent dehydration. Choose water and other clear liquids. If you have kidney, heart, or liver disease and have to limit fluids, talk with your doctor before you increase the amount of fluids you drink.
- When you are able to eat, try clear soups, mild foods, and liquids until all symptoms are gone for 12 to 48 hours. Jell-O, dry toast, crackers, and cooked cereal are also good choices.
- If you have not already done so, prepare a list of advance directives. Advance directives are instructions to your doctor and family members about what kind of care you want if you become unable to speak or express yourself.
Learn more
- Cancer: Controlling Cancer Pain
- Cancer: Controlling Nausea and Vomiting From Chemotherapy
- Cancer: Home Treatment for Constipation
- Cancer: Home Treatment for Diarrhea
- Cancer: Home Treatment for Fatigue
- Cancer: Home Treatment for Mouth Sores
- Cancer: Home Treatment for Pain
- Cancer: Home Treatment for Sleep Problems
- Cancer Support: Managing Stress
- Eating Well During Cancer Treatment
- Hair Loss From Cancer Treatment
Complementary Treatments
Some people use complementary therapies along with medical treatment. They may help relieve the symptoms and stress of cancer or the side effects of cancer treatment. Therapies that may be helpful include:
- Acupuncture to relieve pain and other symptoms.
- Meditation or yoga to relieve stress.
- Massage and biofeedback to reduce pain and tension.
- Breathing exercises to help you relax.
Talk with your doctor about any of these options you would like to try. And let your doctor know if you are already using any complementary therapies. They are not meant to take the place of standard medical treatment. But they may help you feel better and cope better with treatment.
Learn more
Getting Support
Relationships take on new importance when you're faced with cancer. Your family and friends can help support you. You may also want to look beyond those who are close to you.
- Reach out to your family and friends.
Remember that the people around you want to support you, and asking for help isn't a sign of weakness.
- Tell them how they can help.
Your friends and family want to help, but some of them may not know what to do. It may help to make a list. For example, you might ask them to:
- Run errands or pick up kids.
- Deliver meals or groceries to your home.
- Drive you to appointments.
- Go to doctor visits with you and take notes.
- Look for help from other sources.
Places to turn for support include:
- Counseling.
- Counseling can help you cope with cancer and the effect cancer is having on your life. Different types of counseling include family therapy, couples therapy, group counseling, and individual counseling.
- Your health care team.
- Your team should be supportive. Be open and honest about your fears and concerns. Your doctor can help you get the right medical treatments, including counseling.
- Spiritual or religious groups.
- These groups can provide comfort and may be able to help you find counseling or other social support services.
- Social groups.
- Social groups can help you meet new people and get involved in activities you enjoy. Focus on activities that bring you comfort, such as spending time outdoors or being with children.
- A cancer support group.
- Cancer support groups offer support and practical advice. You can hear others talk about:
- What it's like to live with cancer.
- Practical ways to manage your cancer treatment and its side effects.
- Ways to cope with your illness.
Learn more
Related Information
Credits
Current as of: September 25, 2025
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: September 25, 2025
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.




